Tasmar (Oral)
Generic name: tolcapone [ TOLE-ka-pone ]
Drug class: Dopaminergic antiparkinsonism agents
Medically reviewed by Drugs.com. Last updated on Aug 15, 2023.
Because of the risk of potentially fatal, acute fulminant liver failure, tolcapone should ordinarily be used in patients with Parkinson disease on levodopa/carbidopa who are experiencing symptom fluctuations and are not responding satisfactorily to or are not appropriate candidates for other adjunctive therapies. Because of the risk of liver injury and because tolcapone, when it is effective, provides an observable symptomatic benefit, the patient who fails to show substantial clinical benefit within 3 weeks of initiation of treatment, should be withdrawn from tolcapone. Tolcapone therapy should not be initiated if the patient exhibits clinical evidence of liver disease or 2 SGPT/ALT or SGOT/AST values greater than the upper limit of normal. Patients with severe dyskinesia or dystonia should be treated with caution. Patients who develop evidence of hepatocellular injury while on tolcapone and are withdrawn from the drug for any reason may be at increased risk for liver injury if tolcapone is reintroduced. Accordingly, such patients should not ordinarily be considered for retreatment. Cases of severe hepatocellular injury, including fulminant liver failure resulting in death, have been reported in postmarketing use. As of May 2005, 3 cases of fatal fulminant hepatic failure have been reported from more than 40,000 patient-years of worldwide use. This incidence may be 10- to 100-fold higher than the background incidence in the general population. Underreporting of cases may lead to significant underestimation of the increased risk associated with the use of tolcapone. All 3 cases were reported within the first 6 months of initiation of treatment with tolcapone. Analysis of the laboratory monitoring data in over 3400 tolcapone-treated patients participating in clinical trials indicated that increases in SGPT/ALT or SGOT/AST, when present, generally occurred within the first 6 months of treatment with tolcapone .A prescriber who elects to use tolcapone in face of the increased risk of liver injury is strongly advised to monitor patients for evidence of emergent liver injury. Patients should be advised of the need for self-monitoring for both the classical signs of liver disease (eg, clay-colored stools, jaundice) and the nonspecific ones (eg, fatigue, loss of appetite, lethargy). Although a program of periodic laboratory monitoring for evidence of hepatocellular injury is recommended, it is not clear that periodic monitoring of liver enzymes will prevent the occurrence of fulminant liver failure. However, it is generally believed that early detection of drug-induced hepatic injury along with immediate withdrawal of the suspect drug enhances the likelihood for recovery. Accordingly, the following liver monitoring program is recommended. Before starting treatment with tolcapone, the physician should conduct appropriate tests to exclude the presence of liver disease. In patients determined to be appropriate candidates for treatment with tolcapone, serum glutamic-pyruvic transaminase (SGPT/ALT) and serum glutamic-oxaloacetic transaminase (SGOT/AST) levels should be determined at baseline and periodically (ie, every 2 to 4 weeks) for the first 6 months of therapy. After the first 6 months, periodic monitoring is recommended at intervals deemed clinically relevant. Although more frequent monitoring increases the chances of early detection, the precise schedule for monitoring is a matter of clinical judgement. If the dose is increased to 200 mg 3 times a day, liver enzyme monitoring should take place before increasing the dose then be conducted every 2 to 4 weeks for the following 6 months of therapy. After 6 months, periodic monitoring is recommended at intervals deemed clinically relevant. Tolcapone should be discontinued if SGPT/ALT or SGOT/AST exceeds 2 times the upper limit of normal or if clinical signs and symptoms suggest the onset of hepatic dysfunction (persistent nausea, fatigue, lethargy, anorexia, jaundice, dark urine, pruritus, and right upper quadrant tenderness) .
Uses for Tasmar
Tolcapone is used in combination with levodopa and carbidopa for the treatment of the symptoms of Parkinson's disease.
This medicine is available only with your doctor's prescription.
Before using Tasmar
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Studies on this medicine have been done only in adult patients. There is no identified potential use of tolcapone in children.
Geriatric
The risk of hallucinations (seeing, hearing, or feeling things that are not there) may be increased in patients older than 75 years of age.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Iproniazid
- Isocarboxazid
- Levoketoconazole
- Linezolid
- Methotrexate
- Nialamide
- Pargyline
- Pexidartinib
- Phenelzine
- Procarbazine
- Tranylcypromine
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Hallucinations (seeing, hearing, or feeling things that are not there)—Condition may become worse.
- High fever and confusion or
- Muscle injury, aches, cramps—You should not take tolcapone.
- Kidney problems, severe—Elimination of tolcapone may be decreased, which increases the risk of unwanted effects.
- Liver problems or
- Liver tests higher than normal—This medicine can increase chances of serious liver problems. You should not start taking this medicine if you have these problems.
- Low blood pressure or
- Orthostatic or postural low blood pressure (dizziness or lightheadedness when getting up suddenly from a sitting or lying position)—Condition may become worse.
Related/similar drugs
ropinirole, pramipexole, benztropine, carbidopa / levodopa, Exelon, Gocovri
Proper use of Tasmar
Take this medicine only as directed by your doctor, to help your condition as much as possible. Do not take more or less of it, and do not take it more or less often than your doctor ordered.
It is important that you and your doctor discuss the risks of this medicine and that you read and sign a written informed consent before you begin taking this medicine.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For oral dosage form (tablets):
- For Parkinson's disease:
- Adults—100 milligrams (mg) three times a day, taken in addition to levodopa and carbidopa.
- Children—Use and dose must be determined by your doctor.
- For Parkinson's disease:
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Precautions while using Tasmar
It is important that your doctor check your progress at regular visits. Tolcapone may have serious effects on your liver. You must have regular blood tests done to make sure this medicine is not affecting your liver.
Because tolcapone may have serious effects on your liver, you should watch for any signs of these effects. Signs include dark urine; itching; light-colored stools; loss of appetite; nausea (continuing); tenderness in upper right part of abdomen; unusual drowsiness, dullness, or feeling sluggish; unusual tiredness or weakness; or yellow eyes or skin. If you notice any of these signs, contact your doctor.
Do not stop taking tolcapone without first checking with your doctor. Your doctor may want you to gradually reduce the amount you are taking before stopping completely.
Tolcapone may cause dizziness or lightheadedness, drowsiness, weakness, or trouble in thinking or concentrating. Make sure you know how you react to this medicine before you drive, use machines, or do anything else that could be dangerous if you are not alert, well-coordinated, or able to think clearly.
Dizziness, lightheadedness, or fainting may occur, especially when you get up from a lying or sitting position. Getting up slowly may help. If you should have this problem, check with your doctor.
Hallucinations (seeing, hearing, or feeling things that are not there) may occur in some patients. This is more common in elderly patients.
You may experience nausea, especially when you first begin taking this medicine.
Tolcapone causes the urine to turn bright yellow. This is to be expected while you are taking it. This effect is harmless and will go away after you stop taking the medicine.
Side Effects of Tasmar
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
Incidence not known
- Dark urine
- itching
- light-colored stools
- loss of appetite
- nausea (continuing)
- tenderness in upper right part of abdomen
- unusual drowsiness, dullness, or feeling sluggish
- unusual tiredness or weakness
- yellow eyes or skin
Check with your doctor as soon as possible if any of the following side effects occur:
More common
- Abdominal pain
- cough
- diarrhea
- dizziness
- dizziness or lightheadedness when getting up from a lying or sitting position
- drowsiness
- fainting
- fever
- hallucinations (seeing, hearing, or feeling things that are not there)
- headache
- nasal congestion (stuffy nose)
- nausea
- runny nose
- sneezing
- sore throat
- trouble in sleeping
- twitching, twisting, or other unusual body movements
- vomiting
Less common
- Absence of or decrease in body movement
- blood in urine
- chest pain
- chills
- confusion
- falling
- general feeling of discomfort or illness
- hyperactivity
- loss of balance control
- muscle pain
- troubled breathing
Rare
- Agitation
- bloody or cloudy urine
- burning of feet
- burning, prickling, or tingling sensations
- chest discomfort
- difficult or painful urination
- difficulty in thinking or concentrating
- frequent urge to urinate
- irritability
- joint pain, redness, or swelling
- low blood pressure
- muscle cramps
- neck pain
- stiffness
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Constipation
- dryness of mouth
- excessive dreaming
- increased sweating
Less common
- Bleeding
- difficulty in sleeping
- excessive muscle tone
- fever
- heartburn
- gas
- muscle stiffness
- muscle tension or tightness
- trouble in holding or releasing urine
After you stop using this medicine, it may still produce some side effects that need attention. During this period of time, check with your doctor immediately if you notice the following side effects:
- Confusion
- fever
- muscle rigidity
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Commonly used brand name(s)
In the U.S.
- Tasmar
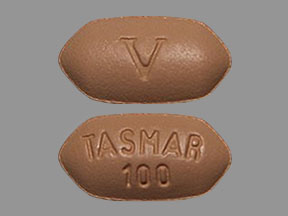
Available Dosage Forms:
- Tablet
Therapeutic Class: Antiparkinsonian
Pharmacologic Class: Catechol-O-Methyltransferase Inhibitor
More about Tasmar (tolcapone)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- Drug class: dopaminergic antiparkinsonism agents
- Breastfeeding
- En español
Patient resources
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.