Ketorolac (Monograph)
Brand name: Sprix
Drug class: Other Nonsteroidal Anti-inflammatory Agents
VA class: CN103
Chemical name: (±)-5-Benzoyl-2,3-dihydro-1H-pyrrolizine-1-carboxylic acid compd. with 2-Amino-2-(hydroxymethyl)-1,3-propanediol (1:1)
Molecular formula: C15H13O3•C4H11NO3
CAS number: 74103-07-4
Warning
- Appropriate Use
-
Parenteral and oral ketorolac indicated for short-term (≤5 days) management of moderately severe acute pain that requires analgesia at opiate level. Oral ketorolac indicated only for continuation therapy and only if necessary; do not exceed 5 days of total parenteral and oral therapy. Not indicated for pediatric use or for use in minor or chronic painful conditions.
-
Increasing the dose beyond the recommended dose will not result in improved efficacy and increases the risk of serious adverse effects.
- GI Effects
-
Can cause peptic ulcers, GI bleeding, and/or perforation,. Contraindicated in patients with active peptic ulcer disease, recent GI bleeding or perforation, or a history of peptic ulcer disease or GI bleeding.
-
Serious GI events can be fatal and can occur at any time and may not be preceded by warning signs and symptoms. Geriatric individuals and patients with history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events. (See GI Effects under Cautions.)
- Cardiovascular Risk
-
Increased risk of serious (sometimes fatal) cardiovascular thrombotic events (e.g., MI, stroke). Risk may occur early in treatment and may increase with duration of use. (See Cardiovascular Thrombotic Effects under Cautions.)
-
Contraindicated in the setting of CABG surgery.
- Renal Effects
-
Contraindicated in patients with advanced renal impairment and those at risk of renal failure because of volume depletion.
- Hematologic Effects
-
Inhibits platelet function. Contraindicated in patients with suspected or confirmed cerebrovascular bleeding, hemorrhagic diathesis, or incomplete hemostasis and in patients at a high risk of bleeding.
-
Contraindicated as prophylactic analgesic before major surgery.
- Sensitivity Reactions
-
Hypersensitivity reactions (e.g., bronchospasm, anaphylactic shock) reported; appropriate counteractive measures must be available when administering the first dose. Contraindicated in patients with known hypersensitivity to ketorolac, aspirin, or other NSAIAs.
- Intrathecal or Epidural Administration
-
Contraindicated for intrathecal or epidural administration because of alcohol content in parenteral formulation.
- Labor and Delivery
-
Contraindicated during labor and delivery. (See Pregnancy under Cautions.)
- Concomitant Use with NSAIAs
-
Contraindicated in patients receiving aspirin or other NSAIAs because of cumulative risk of serious adverse effects.
- Special Populations
-
Adjust dosage in patients ≥65 years of age, adults weighing <50 kg, and those with moderately increased Scr. Daily parenteral dosage should not exceed 60 mg in these patients. (See Dosage and Administration.)
Introduction
Prototypical NSAIA; pyrrolizine carboxylic acid derivative; structurally related to tolmetin and indomethacin.
Uses for Ketorolac
Pain
Consider potential benefits and risks of ketorolac therapy as well as alternative therapies before initiating therapy with the drug. Use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals.
Parenteral ketorolac or sequential parenteral and oral ketorolac: Short-term (i.e., up to 5 days) management of moderately severe, acute pain that requires analgesia at opiate level; mainly used in the postoperative setting.
Intranasal ketorolac: Short-term (i.e., up to 5 days) management of moderate to moderately severe pain that requires analgesia at the opiate level.
Parenteral ketorolac has been used concomitantly with opiate agonist analgesics (e.g., meperidine, morphine) for the management of moderate to severe postoperative pain without apparent adverse drug interactions. Combined use can result in reduced opiate analgesic requirements. (See Syringe Compatibility under Stability.)
Ketorolac Dosage and Administration
General
-
Current principles of pain management indicate that analgesics, including ketorolac, should be administered at regularly scheduled intervals, although the drug also has been administered on an as-needed basis (i.e., withholding subsequent doses until pain returns).
-
Consider potential benefits and risks of ketorolac therapy as well as alternative therapies before initiating therapy with the drug.
Administration
Administer by IM or IV injection, orally, or intranasally.
Switch patients to alternate analgesic therapy as soon as clinically possible.
Oral Administration
Oral formulation is used as continuation therapy only if required following initial parenteral (IV or IM) ketorolac.
Manufacturer makes no specific recommendations regarding administration with meals; high-fat meal may decrease rate but not extent of absorption and reduce peak plasma concentrations.
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Rate of Administration
Administer over ≥15 seconds.
IM Administration
Administer IM slowly and deeply into the muscle.
For drug compatibility information, see Compatibility under Stability.
Intranasal Administration
Administer nasal solution using a metered-dose spray pump. Prime pump prior to initial use. Consult manufacturer's instructions for use of the nasal spray pump.
Not an inhalation product; therefore, patient should not inhale during administration.
Avoid contact with the eyes; if contact occurs, rinse affected eye(s) with water or saline. Patient should consult clinician if ocular irritation persists for >1 hour.
Use each bottle of nasal solution for only 24 hours and then discard; manufacturer states that spray pump will not deliver the intended dose after 24 hours.
Dosage
Available as ketorolac tromethamine; dosage expressed in terms of the salt.
Nasal spray pump delivers 15.75 mg of ketorolac tromethamine per 100-µL metered spray and 8 sprays per single-day bottle.
To minimize the potential risk of adverse cardiovascular and/or GI events, use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals. Adjust dosage based on individual requirements and response; attempt to titrate to the lowest effective dosage.
For breakthrough pain, supplement with low doses of opiate analgesics (unless contraindicated) as needed rather than higher or more frequent doses of ketorolac.
Adults
Pain
Oral
Adults 17–64 years of age: When switching from parenteral to oral therapy, the first oral dose is 20 mg, followed by 10 mg every 4–6 hours as needed (maximum 40 mg in a 24-hour period).
Weight <50 kg: When switching from parenteral to oral therapy, 10 mg every 4–6 hours as needed (maximum 40 mg in a 24-hour period).
IV
30 mg for single-dose therapy. For multiple-dose therapy, 30 mg every 6 hours.
Weight <50 kg: 15 mg for single-dose therapy. For multiple-dose therapy, 15 mg every 6 hours.
IM
60 mg for single-dose therapy. For multiple-dose therapy, 30 mg every 6 hours.
Weight <50 kg: 30 mg for single-dose therapy. For multiple-dose therapy, 15 mg every 6 hours.
Intranasal
31.5 mg (one spray in each nostril) every 6–8 hours (maximum 126 mg [4 doses] daily).
Weight <50 kg: 15.75 mg (one spray in only one nostril) every 6–8 hours (maximum 63 mg [4 doses] daily).
Prescribing Limits
Adults
Pain
Total duration of ketorolac therapy (including parenteral, oral, and intranasal therapy) should not exceed 5 days.
Oral
All adults: Maximum 40 mg in a 24-hour period.
Administer doses no more frequently than every 4–6 hours.
IV or IM
Maximum 120 mg in a 24-hour period.
Weight <50 kg: Maximum 60 mg in a 24-hour period.
Intranasal
Maximum 126 mg (4 doses) daily.
Weight <50 kg: Maximum 63 mg (4 doses) daily.
Special Populations
Hepatic Impairment
Evidence in patients with cirrhosis suggests that dosage adjustment may not be necessary.
Renal Impairment
Pain
Contraindicated in patients with advanced renal disease. Use reduced dosage in those with moderately increased Scr.
Oral
When switching from parenteral to oral therapy, 10 mg every 4–6 hours as needed (maximum 40 mg in a 24-hour period).
IV
15 mg for single-dose therapy. For multiple-dose therapy, 15 mg every 6 hours (maximum 60 mg in a 24-hour period).
IM
30 mg for single-dose therapy. For multiple-dose therapy, 15 mg every 6 hours (maximum 60 mg in a 24-hour period).
Intranasal
15.75 mg (one spray in only one nostril) every 6–8 hours (maximum 63 mg [4 doses] daily).
Geriatric Patients
Adults ≥65 years of age: Use dosage recommended for adults weighing <50 kg and those with moderately increased Scr.
Cautions for Ketorolac
Contraindications
-
Peptic ulcer disease, recent GI bleeding or perforation, or history of peptic ulcer disease or GI bleeding.
-
Advanced renal impairment or risk of renal failure secondary to volume depletion.
-
Labor and delivery.
-
Known hypersensitivity (e.g., anaphylaxis, serious dermatologic reactions) to ketorolac or any ingredient in the formulation.
-
History of asthma, urticaria, or other sensitivity reactions precipitated by aspirin or other NSAIAs.
-
Use as a prophylactic analgesic before major surgery.
-
In the setting of CABG surgery.
-
Suspected or confirmed cerebrovascular bleeding, hemorrhagic diathesis, or incomplete hemostasis; high risk of bleeding.
-
Neuraxial (epidural or intrathecal) administration.
-
Concomitant use with probenecid or pentoxifylline.
-
Manufacturers of oral and parenteral ketorolac also state the drug is contraindicated in patients receiving concomitant aspirin or NSAIA therapy.
Warnings/Precautions
Warnings
Duration of Therapy
Total duration of therapy (including parenteral, oral, and intranasal formulations) should not exceed 5 days.
Cardiovascular Thrombotic Effects
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) increase the risk of serious adverse cardiovascular thrombotic events (e.g., MI, stroke) in patients with or without cardiovascular disease or risk factors for cardiovascular disease.
Findings of FDA review of observational studies, meta-analysis of randomized controlled trials, and other published information indicate that NSAIAs may increase the risk of such events by 10–50% or more, depending on the drugs and dosages studied.
Relative increase in risk appears to be similar in patients with or without known underlying cardiovascular disease or risk factors for cardiovascular disease, but the absolute incidence of serious NSAIA-associated cardiovascular thrombotic events is higher in those with cardiovascular disease or risk factors for cardiovascular disease because of their elevated baseline risk.
Increased risk may occur early (within the first weeks) following initiation of therapy and may increase with higher dosages and longer durations of use.
In controlled studies, increased risk of MI and stroke observed in patients receiving a selective COX-2 inhibitor for analgesia in first 10–14 days following CABG surgery.
In patients receiving NSAIAs following MI, increased risk of reinfarction and death observed beginning in the first week of treatment.
Increased 1-year mortality rate observed in patients receiving NSAIAs following MI; absolute mortality rate declined somewhat after the first post-MI year, but the increased relative risk of death persisted over at least the next 4 years.
Some systematic reviews of controlled observational studies and meta-analyses of randomized studies suggest naproxen may be associated with lower risk of cardiovascular thrombotic events compared with other NSAIAs. FDA states that limitations of these studies and indirect comparisons preclude definitive conclusions regarding relative risks of NSAIAs.
Use NSAIAs with caution and careful monitoring (e.g., monitor for development of cardiovascular events throughout therapy, even in those without prior cardiovascular symptoms) and at the lowest effective dosage for the shortest duration necessary.
Some clinicians suggest that it may be prudent to avoid NSAIA use, whenever possible, in patients with cardiovascular disease. Avoid use in patients with recent MI unless benefits of therapy are expected to outweigh risk of recurrent cardiovascular thrombotic events; if used, monitor for cardiac ischemia. Contraindicated in the setting of CABG surgery.
No consistent evidence that concomitant use of low-dose aspirin mitigates the increased risk of serious adverse cardiovascular events associated with NSAIAs. (See Specific Drugs under Interactions.)
GI Effects
Serious, sometimes fatal, GI toxicity (e.g., bleeding, ulceration, or perforation of esophagus, stomach, or small or large intestine) can occur with or without warning symptoms.
Risk for GI bleeding increased greater than tenfold in patients with a history of peptic ulcer disease and/or GI bleeding who are receiving NSAIAs compared with patients without these risk factors.
Other risk factors for GI bleeding include concomitant use of oral corticosteroids, aspirin, anticoagulants, or SSRIs; longer duration of NSAIA therapy; smoking; alcohol use; older age; poor general health status; and advanced liver disease and/or coagulopathy. (See Contraindications under Cautions.)
Geriatric or debilitated patients appear to tolerate ulceration and bleeding less well than other individuals; most spontaneous reports of fatal GI effects involve such patients.
Use at lowest effective dosage for the shortest duration necessary. Avoid use of more than one NSAIA at a time. (See Specific Drugs under Interactions.)
Avoid use of NSAIAs in patients at higher risk for GI toxicity unless expected benefits outweigh increased risk of bleeding; consider alternate therapies.
NSAIAs may exacerbate inflammatory bowel disease (ulcerative colitis, Crohn's disease); use with great caution in patients with a history of such disease.
Hematologic Effects
May inhibit platelet aggregation and prolong bleeding time. Use with caution and careful monitoring in patients with coagulation disorders. (See Contraindications under Cautions.)
Hematomas and other signs of wound bleeding reported in patients receiving the drug perioperatively; undertake postoperative administration with caution when hemostasis is critical. (See Contraindications under Cautions.)
Increased risk of intramuscular hematoma following IM administration in patients receiving anticoagulants.
Administer with caution in patients receiving therapeutic doses of anticoagulants (e.g., heparin, warfarin). Concurrent use with prophylactic low-dose heparin (2500–5000 units every 12 hours), warfarin, or dextrans not studied extensively, but also may be associated with increased risk of bleeding. Administer with caution when the potential benefits justify the possible risks. (See Specific Drugs under Interactions.)
Increased risk of bleeding following tonsillectomy in pediatric patients.
Renal Effects
Direct renal injury, including renal papillary necrosis, reported in patients receiving long-term NSAIA therapy. Interstitial nephritis and nephrotic syndrome reported in patients receiving ketorolac.
Potential for overt renal decompensation. Increased risk of renal toxicity in patients with renal or hepatic impairment or heart failure; in patients with volume depletion; in geriatric patients; and in those receiving a diuretic, ACE inhibitor, or angiotensin II receptor antagonist. (See Renal Impairment and also Contraindications under Cautions, and Renal Impairment under Dosage and Administration.)
Correct hypovolemia before initiating ketorolac therapy.
Other Warnings and Precautions
Hypertension
Hypertension and worsening of preexisting hypertension reported; either event may contribute to the increased incidence of cardiovascular events. Monitor BP.
Impaired response to ACE inhibitors, angiotensin II receptor antagonists, β-blockers, and certain diuretics may occur. (See Specific Drugs under Interactions.)
Heart Failure and Edema
Fluid retention and edema reported.
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) may increase morbidity and mortality in patients with heart failure.
NSAIAs may diminish cardiovascular effects of diuretics, ACE inhibitors, or angiotensin II receptor antagonists used to treat heart failure or edema. (See Specific Drugs under Interactions.)
Manufacturer recommends avoiding use in patients with severe heart failure unless benefits of therapy are expected to outweigh risk of worsening heart failure; if used, monitor for worsening heart failure.
Some experts recommend avoiding use, whenever possible, in patients with reduced left ventricular ejection fraction and current or prior symptoms of heart failure.
Hypersensitivity Reactions
Anaphylactoid reactions (e.g., anaphylaxis, angioedema) reported. Immediate medical intervention and discontinuance for anaphylaxis.
Avoid in patients with aspirin triad (aspirin sensitivity, asthma, nasal polyps); caution in patients with asthma.
Potentially fatal or life-threatening syndrome of multi-organ hypersensitivity (i.e., drug reaction with eosinophilia and systemic symptoms [DRESS]) reported in patients receiving NSAIAs. Clinical presentation is variable, but typically includes eosinophilia, fever, rash, lymphadenopathy, and/or facial swelling, possibly associated with other organ system involvement (e.g., hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis). Symptoms may resemble those of acute viral infection. Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present in the absence of rash. If signs or symptoms of DRESS develop, discontinue ketorolac and immediately evaluate the patient.
Dermatologic Reactions
Serious skin reactions (e.g., exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis) reported; can occur without warning. Discontinue at first appearance of rash or any other sign of hypersensitivity (e.g., blisters, fever, pruritus).
Hepatic Effects
Severe reactions including jaundice, fatal fulminant hepatitis, liver necrosis, and hepatic failure (sometimes fatal) reported rarely with NSAIAs.
Elevations in ALT or AST reported.
Monitor for symptoms and/or signs suggesting liver dysfunction; monitor abnormal liver function test results. Discontinue ketorolac if associated with abnormal liver function test results.
Other Precautions
Not a substitute for corticosteroid therapy; not effective in the management of adrenal insufficiency.
May mask certain signs of infection or other disease.
Specific Populations
Pregnancy
Use of NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus; use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.
Effects of NSAIAs on the human fetus during third trimester of pregnancy include prenatal constriction of the ductus arteriosus, tricuspid incompetence, and pulmonary hypertension; nonclosure of the ductus arteriosus during the postnatal period (which may be resistant to medical management); and myocardial degenerative changes, platelet dysfunction with resultant bleeding, intracranial bleeding, renal dysfunction or renal failure, renal injury or dysgenesis potentially resulting in prolonged or permanent renal failure, oligohydramnios, GI bleeding or perforation, and increased risk of necrotizing enterocolitis.
Avoid use of NSAIAs in pregnant women at about ≥30 weeks’ gestation; if use required between about 20 and 30 weeks’ gestation, use lowest effective dosage and shortest possible duration of treatment, and consider monitoring amniotic fluid volume via ultrasound examination if treatment duration >48 hours; if oligohydramnios occurs, discontinue drug and follow up according to clinical practice. (See Advice to Patients.)
Fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment observed, on average, following days to weeks of maternal NSAIA use; infrequently, oligohydramnios observed as early as 48 hours after initiation of NSAIAs. Oligohydramnios is often, but not always, reversible (generally within 3–6 days) following NSAIA discontinuance. Complications of prolonged oligohydramnios may include limb contracture and delayed lung maturation. In limited number of cases, neonatal renal dysfunction (sometimes irreversible) occurred without oligohydramnios. Some neonates have required invasive procedures (e.g., exchange transfusion, dialysis). Deaths associated with neonatal renal failure also reported. Limitations of available data (lack of control group; limited information regarding dosage, duration, and timing of drug exposure; concomitant use of other drugs) preclude a reliable estimate of the risk of adverse fetal and neonatal outcomes with maternal NSAIA use. Available data on neonatal outcomes generally involved preterm infants; extent to which risks can be generalized to full-term infants is uncertain.
Animal data indicate important roles for prostaglandins in kidney development and endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, inhibitors of prostaglandin synthesis increased pre- and post-implantation losses; also impaired kidney development at clinically relevant doses.
In animal studies, ketorolac delayed parturition and increased incidence of dystocia. Animal studies conducted during organogenesis revealed no evidence of fetal harm.
Ketorolac may adversely affect fetal circulation and inhibit uterine contractions during labor and delivery, increasing risk of uterine hemorrhage. (See Contraindications under Cautions.)
Lactation
May be distributed into milk in small amounts.
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for ketorolac and any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Although no specific adverse events reported in nursing infants, exercise caution and advise women to contact their infant's clinician if they observe any adverse events.
Fertility
NSAIAs may be associated with reversible infertility in some women. Reversible delays in ovulation observed in limited studies in women receiving NSAIAs; animal studies indicate that inhibitors of prostaglandin synthesis can disrupt prostaglandin-mediated follicular rupture required for ovulation.
Consider withdrawal of NSAIAs in women experiencing difficulty conceiving or undergoing evaluation of infertility.
Pediatric Use
Safety and efficacy of ketorolac (oral, parenteral, or intranasal) not established in pediatric patients <17 years of age. Manufacturer states ketorolac nasal spray should not be used in pediatric patients <2 years of age.
Meta-analysis of data from 13 randomized controlled trials that compared postoperative analgesic efficacy of ketorolac (any dosage and any route of administration) with that of placebo or another active treatment following any type of surgery in pediatric patients up to 18 years of age indicated that available data were inadequate to determine efficacy or assess safety in this population.
Bleeding reported following tonsillectomy. (See Hematologic Effects under Cautions.)
Geriatric Use
Increased risk for serious adverse cardiovascular, GI, and renal effects. Fatal adverse GI effects reported more frequently in geriatric patients than younger adults. Incidence and severity of GI complications increase with increasing dose and duration of therapy.
Substantially excreted by the kidneys; risk of adverse effects may be greater in patients with impaired renal function; because geriatric patients are more likely to have decreased renal function, consider monitoring renal function.
Extreme caution and careful clinical monitoring advised. If anticipated benefits outweigh potential risks, initiate ketorolac at lower end of dosing range; adjust dose and frequency of administration based on response to initial therapy. (See Geriatric Patients under Dosage and Administration.)
Hepatic Impairment
Severe hepatic reactions possible. Use with caution in patients with hepatic impairment or a history of liver disease. (See Hepatic Impairment under Dosage and Administration.)
Renal Impairment
Use with caution in patients with renal impairment or a history of kidney disease since ketorolac is a potent inhibitor of prostaglandin synthesis and the drug and its metabolites are excreted principally by the kidneys; monitor closely. (See Contraindications under Cautions.)
Clearance may be decreased. Dosage adjustment necessary in patients with moderately elevated Scr. (See Renal Impairment under Dosage and Administration.)
Patients with underlying renal insufficiency are at risk of developing acute renal failure; consider risks and benefits before instituting therapy in these patients.
Common Adverse Effects
Oral or parenteral: Headache, somnolence or drowsiness, dizziness, dyspepsia, nausea, GI pain, diarrhea, edema.
Intranasal: Nasal discomfort, rhinalgia, increased lacrimation, throat irritation, oliguria, rash, bradycardia, decreased urine output, increased ALT and/or AST concentration, hypertension, rhinitis.
Drug Interactions
Does not induce or inhibit hepatic enzymes involved in drug metabolism; unlikely to alter its own metabolism of that or other drugs metabolized by CYP isoenzymes.
Protein-bound Drugs
Could be displaced from binding sites by, or could displace from binding sites, some other protein-bound drugs.
Drugs Affecting Hemostasis
Possible increased risk of bleeding complications; carefully monitor patients receiving therapy that affects hemostasis.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitor Possible reversible deterioration of renal function, including acute renal failure, in geriatric patients or patients with volume depletion or renal impairment |
Monitor BP Ensure adequate hydration; assess renal function when initiating concomitant therapy and periodically thereafter Monitor geriatric patients and patients with volume depletion or renal impairment for worsening renal function |
|
Acetaminophen |
No alteration in the protein binding of ketorolac |
|
|
Angiotensin II receptor antagonists |
Reduced BP response to angiotensin II receptor antagonist Possible reversible deterioration of renal function, including acute renal failure, in geriatric patients or patients with volume depletion or renal impairment |
Monitor BP Ensure adequate hydration; assess renal function when initiating concomitant therapy and periodically thereafter Monitor geriatric patients and patients with volume depletion or renal impairment for worsening renal function |
|
Antacids |
No effect on the extent of oral ketorolac absorption |
|
|
Anticonvulsants |
Seizures reported in patients receiving carbamazepine or phenytoin Phenytoin does not alter the protein binding of ketorolac |
|
|
β-Adrenergic blocking agents |
Reduced BP response to β-blocker |
Monitor BP |
|
Cyclosporine |
Possible increased cyclosporine-associated nephrotoxicity |
Monitor for worsening renal function |
|
Dextrans |
Possible increased risk of bleeding |
Carefully monitor patients |
|
Digoxin |
Increased digoxin serum concentrations and prolonged half-life reported No alteration in the protein binding of either drug |
Monitor serum digoxin concentrations |
|
Diuretics (furosemide, thiazides) |
Reduced natriuretic effect Possible increased risk of renal failure due to decreased renal blood flow resulting from prostaglandin inhibition |
Monitor for worsening renal function and for adequacy of diuretic and antihypertensive effects |
|
Fluticasone, intranasal |
Intranasal ketorolac: No change in rate or extent of ketorolac absorption in individuals with symptomatic allergic rhinitis |
|
|
Heparin |
Increased risk of bleeding complications Increased bleeding time when administered with heparin 5000 units; concurrent use with heparin 2500–5000 units sub-Q every 12 hours not studied extensively |
Extreme caution advised in patients receiving therapeutic doses of heparin; carefully monitor patients |
|
Lithium |
Increased plasma lithium concentrations |
Monitor for lithium toxicity |
|
Methotrexate |
Increased plasma methotrexate concentrations in patients receiving other NSAIAs; studies with ketorolac have not been undertaken |
Monitor for methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction) |
|
Nondepolarizing skeletal muscle relaxants |
May potentiate the effects of the muscle relaxant resulting in apnea |
Monitor for apnea |
|
NSAIAs |
Concomitant NSAIAs and aspirin (analgesic dosages): Therapeutic effect not greater than that of NSAIAs alone; increased risk for bleeding and serious GI events Aspirin: No consistent evidence that low-dose aspirin mitigates the increased risk of serious cardiovascular events associated with NSAIAs Therapeutic anti-inflammatory concentrations of salicylates (300 mcg/mL) may displace ketorolac from binding sites; ibuprofen, naproxen, or piroxicam does not alter the protein binding of ketorolac Protein binding of NSAIAs reduced by aspirin, but clearance of unbound NSAIA not altered; clinical importance unknown |
Concomitant use of ketorolac and analgesic dosages of aspirin generally not recommended; manufacturers of oral and parenteral ketorolac state concomitant use with aspirin or other NSAIAs is contraindicated Advise patients receiving ketorolac not to take low-dose aspirin without consulting clinician; closely monitor patients receiving concomitant antiplatelet agents, including aspirin, for bleeding |
|
Oxymetazoline, intranasal |
Intranasal ketorolac: No change in rate or extent of ketorolac absorption in individuals with symptomatic allergic rhinitis |
|
|
Pemetrexed |
Possible increased risk of pemetrexed-associated myelosuppression, renal toxicity, and GI toxicity |
Short half-life NSAIAs (e. g., diclofenac, indomethacin): Avoid beginning 2 days before and continuing through 2 days after pemetrexed administration Longer half-life NSAIAs (e.g., meloxicam, nabumetone): In the absence of data, avoid beginning at least 5 days before and continuing through 2 days after pemetrexed administration Patients with Clcr 45–79 mL/minute: Monitor for myelosuppression, renal toxicity, and GI toxicity |
|
Pentoxifylline |
Increased risk of bleeding |
Concomitant use contraindicated |
|
Probenecid |
Increased plasma concentrations and AUC of ketorolac |
Concomitant use contraindicated |
|
Psychotherapeutic agents (e.g., fluoxetine, thiothixene, alprazolam) |
Hallucinations reported |
Monitor for hallucinations |
|
Serotonin-reuptake Inhibitors (e.g., SSRIs, SNRIs) |
Possible increased risk of bleeding due to importance of serotonin release by platelets in hemostasis |
Monitor for bleeding |
|
Thrombolytic agents |
Possible increased risk of bleeding |
Carefully monitor patients |
|
Tolbutamide |
No alteration in the protein binding of ketorolac |
|
|
Warfarin |
Increased risk of bleeding complications; concurrent use not studied extensively Possible slight displacement of warfarin (but not ketorolac) from binding sites; other pharmacokinetic interactions unlikely |
Extreme caution advised in patients receiving therapeutic doses of warfarin; carefully monitor patients |
Ketorolac Pharmacokinetics
Absorption
Bioavailability
IM: Rapidly and completely absorbed.
Oral: Rapidly and almost completed absorbed; bioavailability reported to be 80–100%.
Intranasal: Bioavailability approximately 60% compared with IM injection. Peak concentrations achieved at about 45 minutes. Presence of allergic rhinitis does not substantially alter pharmacokinetics.
Onset
IM administration: Onset in 10 minutes, with peak analgesia at 75–150 minutes.
Oral administration: Onset in 30–60 minutes, with peak analgesia at 1.5–4 hours.
Duration
Oral or IM administration: 6–8 hours.
Food
Food decreases rate but not extent of absorption.
Special Populations
Rate of absorption from GI tract may be decreased in patients with hepatic or renal impairment and in geriatric individuals.
Distribution
Extent
Not distributed widely. Crosses the blood-brain barrier poorly.
Crosses the placenta; distributed into milk.
Intranasal: Most of dose is deposited in nasal cavity and pharynx; <20% is deposited in esophagus and stomach, and <0.5% is deposited in lungs.
Plasma Protein Binding
>99%.
Elimination
Metabolism
Metabolized in the liver by hydroxylation; also undergoes conjugation with glucuronic acid.
Elimination Route
Excreted in urine (92%) as parent drug (60%) or metabolites (40%) and in feces (6%).
Half-life
4–6 hours in adults; 3.8–6.1 hours in pediatric patients.
Special Populations
Hepatic impairment (e.g., cirrhosis) does not appear to substantially affect half-life. In patients with cirrhosis, half-life of about 4.5–5.4 hours reported.
Renal impairment: Half-life is about 9–10 hours (range: 3.2–19 hours); in patients undergoing dialysis, half-life of about 13.6 hours (range: 8–39.1 hours) reported.
Geriatric individuals: Half-life is about 5–7 hours (range: 4.3–8.6 hours).
Stability
Storage
Nasal
Solution
Unopened: 2–8°C; protect from light and freezing. During use: 15–20°C out of direct sunlight. Discard within 24 hours after priming the spray pump.
Oral
Tablets
15–30°C.
Parenteral
Injection
15–30°C; protect from light.
Compatibility
Parenteral
Solution Compatibility212
|
Compatible |
|---|
|
Dextrose 5% in sodium chloride 0.9% |
|
Dextrose 5% in water |
|
Plasma-Lyte A, pH 7.4 |
|
Ringer’s injection |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Incompatible |
|---|
|
Cyclizine lactate |
|
Haloperidol lactate |
|
Hydroxyzine HCl |
|
Meperidine HCl |
|
Morphine Sulfate |
|
Nalbuphine |
|
Prochlorperazine edisylate |
|
Promethazine HCl |
|
Variable |
|
Diazepam |
|
Hydromorphone HCl |
Ketorolac tromethamine 1 mg/mL tested.
|
Compatible |
|---|
|
Acetaminophen |
|
Dexmedetomidine HCl |
|
Fentanyl citrate |
|
Hetastarch in lactated electrolyte injection (Hextend) |
|
Hydromorphone HCl |
|
Methadone HCl |
|
Morphine sulfate |
|
Remifentanil HCl |
|
Incompatible |
|
Azithromycin |
|
Fenoldopam mesylate |
|
Variable |
|
Cisatracurium besylate |
Actions
-
Inhibits cyclooxygenase-1 (COX-1) and COX-2.
-
Pharmacologic actions similar to those of other prototypical NSAIAs; exhibits anti-inflammatory, analgesic, and antipyretic activity.
Advice to Patients
-
Importance of reading the medication guide for NSAIAs that is provided each time the drug is dispensed.
-
Risk of serious cardiovascular events (e.g., MI, stroke). Importance of seeking immediate medical attention if signs and symptoms of a cardiovascular event (e.g., chest pain, dyspnea, weakness, slurred speech) occur.
-
Risk of GI bleeding and ulceration. Importance of notifying clinician if signs and symptoms of GI ulceration or bleeding develop.
-
Risk of bleeding following tonsillectomy.
-
Risk of serious skin reactions, DRESS, and anaphylactic and other sensitivity reactions. Advise patients to stop taking ketorolac immediately if they develop any type of rash or fever and to promptly contact their clinician. Importance of seeking immediate medical attention if an anaphylactic reaction occurs.
-
Risk of hepatotoxicity. Importance of discontinuing therapy and contacting clinician immediately if signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, upper right quadrant tenderness, flu-like symptoms) occur.
-
Risk of kidney failure.
-
Risk of heart failure or edema; importance of reporting dyspnea, unexplained weight gain, or edema.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of avoiding NSAIA use beginning at 20 weeks’ gestation unless otherwise advised by a clinician; importance of avoiding NSAIAs beginning at 30 weeks’ gestation because of risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy required for >48 hours’ duration between about 20 and 30 weeks’ gestation.
-
Advise women who are trying to conceive that NSAIAs may be associated with a reversible delay in ovulation.
-
Importance of not exceeding recommended duration of therapy.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Nasal |
Solution |
15.75 mg/metered spray |
Sprix |
Zyla |
|
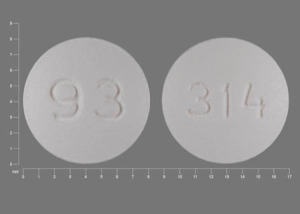
Oral |
Tablets, film-coated |
10 mg* |
Ketorolac Tromethamine Tablets |
|
|
Parenteral |
Injection, for IM or IV use |
15 mg/mL* |
Ketorolac Tromethamine Injection |
|
|
30 mg/mL* |
Ketorolac Tromethamine Injection |
|||
|
Injection, for IM use |
30 mg/mL* |
Ketorolac Tromethamine Injection |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions October 18, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
- How and where is the Toradol injection given?
- Which painkiller should you use?
- How long does ketorolac (Toradol) stay in your system?
More about ketorolac
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (458)
- Drug images
- Latest FDA alerts (10)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding
Patient resources
Professional resources
- Ketorolac prescribing information
- Ketorolac Injection (FDA)
- Ketorolac Tromethamine (FDA)
- Ketorolac Tromethamine Nasal Spray (FDA)